Hello to my patient family. I wanted to apologize for a long hiatus from writing the Dental Newsletter. As many of you now know, Dr. Krist has officially retired and is enjoying the next two months in Tuscany celebrating his 43 year career with friends and family. Our practice transition has been running very smoothly over the past three years and it is my honor to continue the legacy of this dental practice. I hope to have a long and fulfilling career, as Dr. Krist did, providing patients with the highest level of care, skill and judgement.
To all of those who read this newsletter, thank you. I hope you find this practice newsletter educational and interesting; perhaps it may even answer some questions about oral health that you may have been pondering. If you have any dental questions or topics you would like me to write about, please let me know! This newsletter will be about gum recession, its causes, and a pathway of clinical decision making.
In order to understand gum recession, we must understand the anatomy of the gums. There are two main tissue types when we are talking about gums: attached keratinized tissue and mucosa. Attached tissue is firm, lighter in color, and attached to underlying bone. Mucosa is moveable, darker in color, and is more loosely attached to the cheeks and lips.
Gum recession occurs for many different reasons and is irreversible once it occurs. When gum recession occurs, the roots of our teeth become exposed and the tooth is no longer protected by enamel on the root. The roots of our teeth have free nerve endings which can cause painful hypersensitivity to hot and cold stimuli. Our mutual clinical goal as doctor and patient should be to preserve attached gingiva because it protects the bone and roots of our teeth. Mucosa is much more fragile and sensitive to irritation. Here are some of the main causes of attached tissue gum recession:
- Brushing Too Hard: This may be the most common cause and it is a result of poor tooth brushing technique. Sometimes people try to “scrub” their teeth and use too much pressure and vigorous brush strokes which slowly but surely recede the gums away.
- Gum Disease: Chronic inflammation of the gums from poor oral hygiene and poorly contoured restorations eventually leads to recession of the gums and underlying bone.
- Clenching and Grinding: Squeezing our teeth together causes flexure of the teeth and underlying bone. This continual flexure causes degradation of the teeth and bone and the gums recede in response.
- Drifting Teeth and Inappropriate Forces: Forces to teeth cause them to move and can push the teeth out of the envelope of bone in the jaw. We can intentionally apply forces to teeth with orthodontics to align teeth or unintentionally apply forces to teeth through everyday function. When teeth are pushed outside of their bony envelope, the attached tissue recedes.
- Congenital Muscle Attachment: We have a piece of muscle called a “frenum” that attaches the gums to the cheeks, tongue, and lips at several points in our mouth. If the frenum attachment to the gums is pulling too hard, it can cause recession.
Although gum recession is irreversible, it can be managed by patients and their dental healthcare providers. Here are the main treatments for combating and preventing gum recession:
- Gum Grafting: This is the gold standard for combating gum recession. There are many different types of grafts and grafting materials. I do not perform gum grafts so I refer this procedure to a periodontist. It is always worth having a consultation with a periodontist to discuss the pros, cons, and expectations to understand if a graft makes sense in a situation of recession.
- Orthodontics: It can be helpful to move teeth via braces or Invisalign into a more harmonious bite pattern if a patient has a traumatic bite pattern that is causing destructive forces to the gums, teeth, and underlying bone.
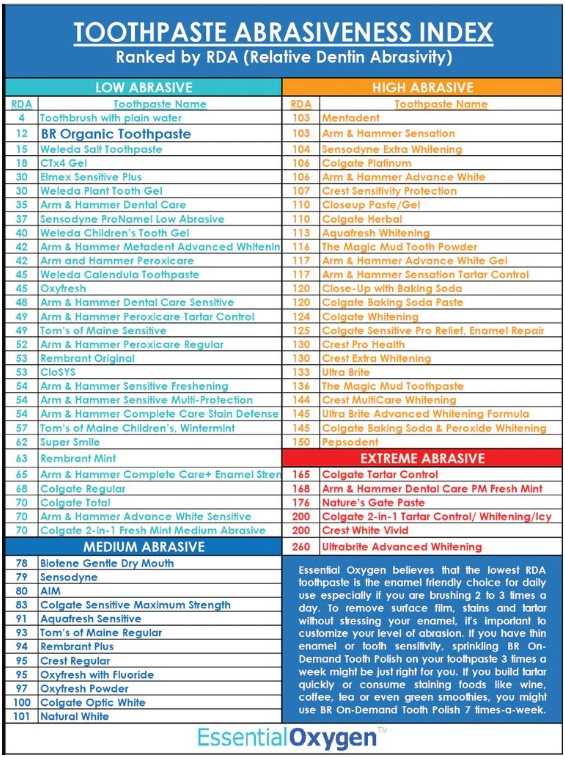
- Modifying Brushing Technique: This is often the easiest change patients can make to stop recession. It involves using an extra soft bristled electric toothbrush, soft toothpaste found from the RDA toothpaste abrasiveness chart (included below), appropriate amount of pressure when pressing down with your toothbrush, and the correct brushstrokes. Angle your toothbrush at a 45 degree angle toward the gum line and allow the toothbrush to do the work for you. A heavy handed “scrubbing” motion is never needed, small gentle circular brush strokes are best. Change your brush head frequently enough so that the bristles are not frayed and splayed out.
- Active Surveillance: We will measure your gum recession on a yearly basis to make sure that it is not progressing. If the numbers are changing in a negative trend then we will discuss the most logical next steps to protect the gums.
- Night Guard: A night guard can help minimize damage to our teeth from repeated episodes of grinding in our sleep. Behavior modification helps minimize damage from grinding during the day.
- Frenectomy: Sometimes a frenum that is pulling too hard on the gums needs to be snipped back a little bit to prevent further recession.
- Composite Bonding: I can add composite bonding to areas of the root that are exposed by gum recession as a last case scenario if patients refuse grafting and have cosmetic concerns or prolonged hypersensitivity to thermal stimuli.
I hope this has been educational and helpful! As always, if you have any questions or concerns, I am always a phone call away.
With care,
Dr. Obeck